COVID in Prisons - It's Not Done With Us Yet
"Left alone & without attention is like a torture chamber for the sick and old.”

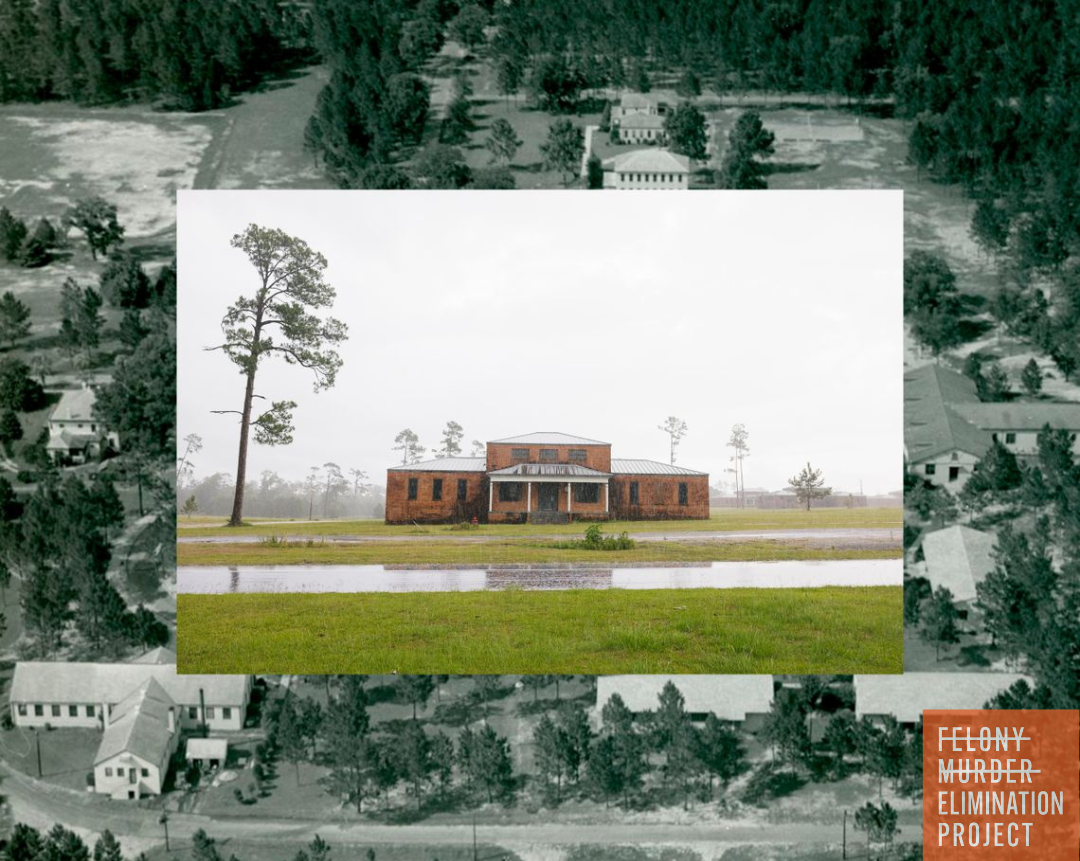
On April 3, 2020, after five COVID deaths in the federal prison in Oakdale, Louisiana, U.S. Attorney General William Barr directed the Bureau of Prisons to ordering a review of “all inmates who have COVID-19 risk factors.” Two days later, he declared an emergency in the federal system, giving prison officials the power to grant early release beyond the 10 percent remaining sentence or six months, whichever was less, as was specified in the First Step Act of 2019. By August of 2020, federal authorities stated they had released over 30,000 people, the largest mass release in U.S. prison history. The vast majority were placed on house arrest with an electronic monitor.
Despite the myriad of excessive restrictions and intrusions placed on home confinement, many released able to rebuild their lives. After two years, out of 11,000 persons released under the CARES Act, only 17 people were returned to prison for new criminal charges. This proved that authorities could successfully release people and communities could still be safe, as there are community outlets and support services that could be utilized to keep people on the outside who remained law-abiding and productive members of their communities.
For those that remained in prison, torturous conditions and lockdowns were used to stop the spread of COVID. These COVID-related lockdowns lead to oppressive conditions often identical to traditional forms of solitary confinement, such as administrative segregation (used for people whom the prison labels a security risk) and disciplinary segregation (used as punishment for rule infractions). Solitary Watch noted a 500 percent increase in the use of solitary confinement across the country, as facilities scrambled to slow the spread of the virus.
By now, prison officials and politicians have had more than two years to adapt and learn from mistakes — and to heed medical advice to significantly depopulate prisons and jails, but have failed to do so. Behind bars, COVID is far from a done deal.
These widespread lockdowns force hundreds of thousands of incarcerated people throughout the country to survive with limited access to programming, visitation, medical and mental health care, recreation, showers, law libraries, adequate food and commissary (in-facility stores selling food, hygiene supplies and other necessities), turning the already miserable experience of incarceration into torture. Despite these countless lockdowns, COVID remains rampant behind bars, resulting in the death of over 2,900 incarcerated persons, 279 prison staff, 633,000 infections of incarcerated people and 233,000 infected staff, as tracked by the COVID Prison Project.
Many carceral facilities have failed to implement other medically recommended COVID-19 precautions, such as increasing testing, placing people into mini-communities, enforcing staff vaccine mandates, and creating healthier spaces for medical isolation that do not resemble solitary confinement.
Leonard Peltier, a 77-year-old Native American rights activist, wrote a letter to the Huffington Post in January about how conditions were even worse than last year’s lockdowns in USP Coleman I, a federal prison in Florida. “In and out of lockdown last year at least meant a shower every third day, a meal beyond a sandwich wet with a little peanut butter,” he wrote. “But now with COVID for an excuse, nothing. No phone, no window, no fresh air — no humans to gather — no loved one’s voice. No relief. Left alone and without attention is like a torture chamber for the sick and old.”
Recidivism rates were non-existent among those released to home confinement during the first waves of COVID in 2020. To reiterate; out of 11,000 people released, 17 returned to prison, a 0.15 percent recidivism rate in a country where it’s normal for 30 to 65 percent of people coming home from prison to reoffend within three years of release.
COVID isn't done with us, and the policies enacted to keep incarcerated persons safe - the community at highest risk for transmission and represents the largest outbreaks since the start of the pandemic - should remain active as well.